Healthcare Fraud Analytics Market Report Scope & Overview:
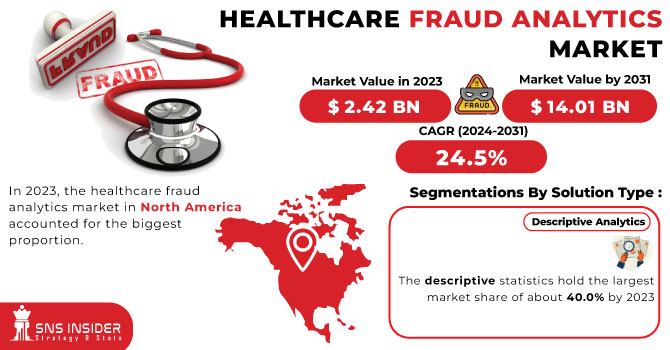
Healthcare Fraud Analytics Market Size was valued at USD 2.36 Billion in 2023 and is expected to reach USD 17.6 Billion by 2032, growing at a CAGR of 25% over the forecast period 2024-2032. The Healthcare Fraud Analytics Market Report provides valuable information on the detection rates of fraud, financial losses, key drivers of the market, and the increasing adoption of AI and machine learning. It provides breakdowns of types of fraud and frequency by region, with emphasis on billing fraud, identity theft, and false claims. Furthermore, the report assesses the investments in fraud analytics solutions over time across the public and private sectors and also assesses the effect of regulatory compliance (HIPAA, GDPR) on fraud detection. The new report also compares cloud-based vs. on-premise fraud analytics adoption, illustrating the overall shift of the industry towards advanced, scalable fraud detection technologies. The healthcare fraud analytics market is driven by the increasing sophistication of fraudulent activities in the healthcare sector.
Get more information on Healthcare Fraud Analytics Market - Request Sample Report
Market Dynamics
Drivers
-
The increasing prevalence of fraudulent activities in the healthcare sector necessitates advanced analytics solutions for effective detection and prevention.
The rising occurrence of healthcare fraud has become a major issue and has led to the implementation of advanced analytics solutions for efficient detection and prevention. In Q1 2024, Americans lost more than USD 16 million to numerous healthcare fraud schemes-as the Federal Trade Commission (FTC) received 16,396 fraud reports, 53% of which reported losing money. The median loss per incident was USD 258, with most fraudulent activities being made via calls and payments via credit cards. Florida emerged as a hotspot, contributing 1,562 complaints during this period. A particularly worrisome trend is the rise of fraudulent medical treatments and cures. In the first quarter of 2024, losses in this category amounted to USD 12 million, a staggering 1,100 percent increase compared to the same quarter last year. Such a sharp increase highlights the critical need for strong fraud detection mechanisms to protect consumers against fraudulent medical claims. Moreover, systemic issues such as "ghost networks" exacerbate the problem. A class-action lawsuit filed in November 2024 accused Anthem Blue Cross Blue Shield of New York of maintaining inaccurate directories of mental health providers. Investigations revealed that out of 100 listed providers, only seven were available for appointments, highlighting the deceptive practices that hinder patient access to legitimate care.
Restraint:
-
Handling sensitive patient information requires robust data protection measures, posing challenges in the implementation of fraud analytics solutions.
Data privacy and security concerns significantly hinder the adoption of healthcare fraud analytics solutions. The healthcare sector has become a prime target for cyberattacks, with 84% of organizations experiencing at least one incident in the past year. These breaches often lead to severe financial repercussions, as evidenced by the average cost of a healthcare data breach reaching USD 9.8 million in 2024. The sensitivity of protected health information (PHI) exacerbates these concerns, as unauthorized access can result in identity theft, financial fraud, and compromised patient trust. For instance, in 2024, hacking and IT incidents accounted for 81.2% of large healthcare data breaches, exposing over 259 million records. The implementation of fraud analytics necessitates access to vast amounts of sensitive data, raising fears about potential vulnerabilities and unauthorized disclosures. Consequently, healthcare organizations may hesitate to adopt these solutions, prioritizing the protection of patient information over the integration of advanced analytics tools. This cautious approach underscores the critical need for robust security measures and compliance with stringent data protection regulations to foster trust and facilitate the adoption of fraud analytics in the healthcare industry.
Opportunity:
-
Innovations in artificial intelligence and machine learning enhance the capabilities of fraud detection systems, offering more efficient and accurate identification of fraudulent activities.
AI and ML are also used for healthcare fraud detection, as monitoring searches for anomalies in the data ensures a consistently high level of performance. Recent innovation has shown that AI-based solutions are feasible here. Moreover, the U.S. Department of Justice's Fraud Section reported a substantial increase in enforcement actions in 2024, charging 234 individuals and securing 252 convictions related to healthcare fraud. This increase can be partly attributed to the adoption of advanced data analytics and AI technologies that have improved the ability to detect and prosecute complex fraud schemes.
According to the National Health Care Anti-Fraud Association, healthcare fraud accounts for as much as USD 68 billion a year in costs to the U.S. industry. Adopting AI-powered fraud detection tools led to a 30% decrease in false positives and a 45% increase in detection accuracy. These statistics demonstrate the financial and operational advantages of implementing AI technologies in the fight against healthcare fraud. These developments illustrate the transformative impact of AI and ML in healthcare fraud detection, offering robust tools to identify and prevent fraudulent activities, thereby safeguarding financial resources and ensuring compliance within the healthcare system.
Challenge:
-
Incorporating advanced fraud analytics into existing healthcare infrastructures can be complex due to compatibility issues with outdated systems.
The lack of governance mechanisms, however, such as Healthcare data privacy and security, is one of the major challenges in adopting Healthcare Fraud Analytics Solutions. The healthcare sector has been singled out as a key target of cyberattacks with 84% of organizations reporting that they had at least one incident during the last year. Such breaches often carry heavy financial penalties in 2024, the average cost of a healthcare data breach was USD 9.8 million. These challenges are particularly problematic because of the sensitivity of protected health information (PHI) unauthorized access which can cause identity theft, financial fraud, and violate patient trust. For example, in 2024, hacking & IT incidents represented 81.2% of large-scale healthcare data breaches, exposing more than 259 million records. As part of implementing fraud analytics, there will be potential access to huge amounts of sensitive data that can spark fears of destroyed integrity and unauthorized disclosures. As a result, healthcare organizations might be reluctant to implement these solutions, putting more emphasis on safeguarding patient information than utilizing cutting-edge analytics solutions. This prudential stance emphasizes the necessity of stringent security protocols and adherence to rigorous data privacy laws to ensure confidence and encourage the implementation of fraud analytics in healthcare.
Segment Analysis
By Solution Type
In 2023, the descriptive analytics segment accounted for the largest market share, over 39%. The popularity of this method can be attributed to several reasons, such as its capability to give an overview of historical information as well as spotting patterns that can help characterize fraudulent activities. Through descriptive analytics, healthcare organizations can gain valuable insights into historical trends and past behaviours so that anomalies and potential fraud can be detected in a more timely manner. In fiscal year 2023, the U.S. Centers for Medicare & Medicaid Services (CMS) said descriptive analytics found USD 1.87 billion in improper payments through its Fraud Prevention System (FPS). The figures above show a significant increase over previous years and a maturing in the value that descriptive analytics can provide for fraud detection.
Additionally, the U.S. Department of Health and Human Services’ Office of Inspector General (OIG) reported that descriptive analytics were key in identifying 1,648 providers for fraud investigations in 2023. This resulted in 324 law enforcement actions and the recovery of USD 496 million in fraudulent claims. Because descriptive analytics is more accessible and interpretable than other statistical methods, it can be adopted by healthcare organizations of any size. Its ability to provide clear, actionable insights without requiring advanced statistical knowledge has contributed to its widespread adoption across the industry.
By Delivery Model
In 2023, the on-premise segment held the majority of revenue share 52%. This remarkable market share can be primarily ascribed to various factors including the improved security and control of on-premise solutions that aid healthcare organizations in handling sensitive patient data accompanied by financial information. In 2023, 713 healthcare data breaches involving more than 51 million individuals occurred, according to the Office for Civil Rights within the U.S. Department of Health and Human Services. This one statistic highlights the need for strong data security measures within the healthcare space. On-premise solutions offer organizations extensive control over their data and security protocols, which is critical when working with personal healthcare information and fraud detection operations.
In 2023, healthcare-related cybersecurity crimes caused over USD 4.6 billion in losses, according to the Federal Bureau of Investigation (FBI). Such exorbitant figures have led to a focus for many healthcare organizations to prioritize on-premise solutions that provide additional security features and compliance with strict data protection regulations, including HIPAA. Furthermore, the U.S. Government Accountability Office (GAO) found that federal agencies and organizations within the healthcare sector are increasingly choosing to deploy on-premise solutions for vital systems so that they can maintain direct control of their data and minimize exposure to outside threats. This further contributes to the market share of on-premise delivery models in the healthcare fraud analytics market.
By Application
The insurance claims review segment held the largest market share of over 35% in 2023. This significant market share can be attributed to the critical role that insurance claims review plays in detecting and preventing healthcare fraud, waste, and abuse. According to the National Health Care Anti-Fraud Association (NHCAA), the United States loses tens of billions of dollars to healthcare fraud each year. The Centers for Medicare & Medicaid Services (CMS) reported that in fiscal year 2023, improper payments in Medicare Fee-for-Service (FFS) programs amounted to USD 31.6 billion, representing an improper payment rate of 7.7%. This staggering figure highlights the urgent need for robust insurance claims review processes.
The U.S. Department of Justice (DOJ) reported that in 2023, it recovered over USD 1.8 billion from healthcare fraud cases related to false claims submitted to federal healthcare programs. This statistic underscores the effectiveness of advanced analytics in identifying and investigating fraudulent insurance claims. Furthermore, the Office of Inspector General (OIG) of the Department of Health and Human Services stated that their use of advanced analytics in claims review led to the identification of USD 3.2 billion in expected investigative recoveries in fiscal year 2023. This demonstrates the significant financial impact of implementing sophisticated insurance claims review processes.
By End-user
Public & government organizations accounted for the largest share of more than 41.0% of the healthcare fraud analytics market in 2023. The substantial market share can be linked to the large-scale media commitment by government organizations to prevent misuse of social security and other health programs against monetary loss. According to the CMS Report for Fiscal Year 2023, the CMS Fraud Prevention System (FPS) identified or prevented $1.87 billion in improper payments. As public agencies have started using this sophisticated analytics system, this is proof that the government is committed to using cutting-edge technologies for fraud detection as well as prevention.
The U.S. Department of Health and Human Services Office of Inspector General (HHS-OIG) released a report stating that their investigative enforcement activity in 2023 led to a total of 1,648 criminal actions against individuals or entities whose actions violated Medicare and Medicaid. They also excluded 3,005 individuals and entities from participation in Federal health care programs. They also show the power of fraud analytics used by government agencies to detect and prevent fraud. In addition, the Department of Justice (DOJ) reported that it secured over USD 2.68 billion in settlements and judgments in civil cases involving fraud and false claims against the government during the fiscal year 2023. Almost half of these recovery actions were related to healthcare fraud, demonstrating the important role of public agencies in using fraud analytics to combat cheating in government healthcare programs.
Segment Analysis
By Solution Type
In 2023, the descriptive analytics segment accounted for the largest market share, over 39%. The popularity of this method can be attributed to several reasons, such as its capability to give an overview of historical information as well as spotting patterns that can help characterize fraudulent activities. Through descriptive analytics, healthcare organizations can gain valuable insights into historical trends and past behaviours so that anomalies and potential fraud can be detected in a more timely manner. In fiscal year 2023, the U.S. Centers for Medicare & Medicaid Services (CMS) said descriptive analytics found USD 1.87 billion in improper payments through its Fraud Prevention System (FPS). The figures above show a significant increase over previous years and a maturing in the value that descriptive analytics can provide for fraud detection.
Additionally, the U.S. Department of Health and Human Services’ Office of Inspector General (OIG) reported that descriptive analytics were key in identifying 1,648 providers for fraud investigations in 2023. This resulted in 324 law enforcement actions and the recovery of USD 496 million in fraudulent claims. Because descriptive analytics is more accessible and interpretable than other statistical methods, it can be adopted by healthcare organizations of any size. Its ability to provide clear, actionable insights without requiring advanced statistical knowledge has contributed to its widespread adoption across the industry.
By Delivery Model
In 2023, the on-premise segment held the majority of revenue share 52%. This remarkable market share can be primarily ascribed to various factors including the improved security and control of on-premise solutions that aid healthcare organizations in handling sensitive patient data accompanied by financial information. In 2023, 713 healthcare data breaches involving more than 51 million individuals occurred, according to the Office for Civil Rights within the U.S. Department of Health and Human Services. This one statistic highlights the need for strong data security measures within the healthcare space. On-premise solutions offer organizations extensive control over their data and security protocols, which is critical when working with personal healthcare information and fraud detection operations.
In 2023, healthcare-related cybersecurity crimes caused over USD 4.6 billion in losses, according to the Federal Bureau of Investigation (FBI). Such exorbitant figures have led to a focus for many healthcare organizations to prioritize on-premise solutions that provide additional security features and compliance with strict data protection regulations, including HIPAA. Furthermore, the U.S. Government Accountability Office (GAO) found that federal agencies and organizations within the healthcare sector are increasingly choosing to deploy on-premise solutions for vital systems so that they can maintain direct control of their data and minimize exposure to outside threats. This further contributes to the market share of on-premise delivery models in the healthcare fraud analytics market.
By Application
The insurance claims review segment held the largest market share of over 35% in 2023. This significant market share can be attributed to the critical role that insurance claims review plays in detecting and preventing healthcare fraud, waste, and abuse. According to the National Health Care Anti-Fraud Association (NHCAA), the United States loses tens of billions of dollars to healthcare fraud each year. The Centers for Medicare & Medicaid Services (CMS) reported that in fiscal year 2023, improper payments in Medicare Fee-for-Service (FFS) programs amounted to USD 31.6 billion, representing an improper payment rate of 7.7%. This staggering figure highlights the urgent need for robust insurance claims review processes.
The U.S. Department of Justice (DOJ) reported that in 2023, it recovered over USD 1.8 billion from healthcare fraud cases related to false claims submitted to federal healthcare programs. This statistic underscores the effectiveness of advanced analytics in identifying and investigating fraudulent insurance claims. Furthermore, the Office of Inspector General (OIG) of the Department of Health and Human Services stated that their use of advanced analytics in claims review led to the identification of USD 3.2 billion in expected investigative recoveries in fiscal year 2023. This demonstrates the significant financial impact of implementing sophisticated insurance claims review processes.
By End-user
Public & government organizations accounted for the largest share of more than 41.0% of the healthcare fraud analytics market in 2023. The substantial market share can be linked to the large-scale media commitment by government organizations to prevent misuse of social security and other health programs against monetary loss. According to the CMS Report for Fiscal Year 2023, the CMS Fraud Prevention System (FPS) identified or prevented $1.87 billion in improper payments. As public agencies have started using this sophisticated analytics system, this is proof that the government is committed to using cutting-edge technologies for fraud detection as well as prevention.
The U.S. Department of Health and Human Services Office of Inspector General (HHS-OIG) released a report stating that their investigative enforcement activity in 2023 led to a total of 1,648 criminal actions against individuals or entities whose actions violated Medicare and Medicaid. They also excluded 3,005 individuals and entities from participation in Federal health care programs. They also show the power of fraud analytics used by government agencies to detect and prevent fraud. In addition, the Department of Justice (DOJ) reported that it secured over USD 2.68 billion in settlements and judgments in civil cases involving fraud and false claims against the government during the fiscal year 2023. Almost half of these recovery actions were related to healthcare fraud, demonstrating the important role of public agencies in using fraud analytics to combat cheating in government healthcare programs.
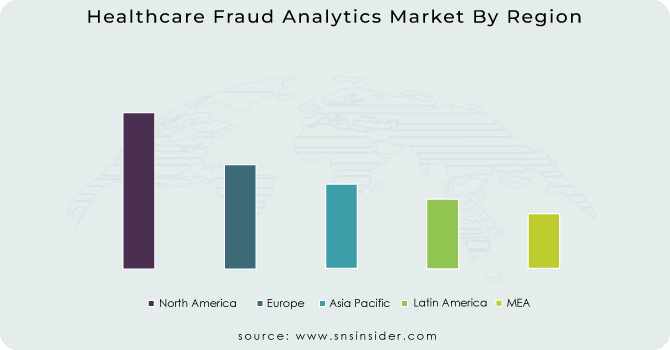
Regional Analysis
In 2023, North America held the largest market share of healthcare fraud analytics, accounting for around 39% of the total market share. The dominance can be ascribed to the region's advanced healthcare infrastructure, high adoption rate of digital health technologies, and stringent regulatory environment. In particular, the United States has served as a pioneer in the deployment of methods for the analytics of healthcare fraud. In the United States, recoveries from healthcare fraud investigations totaled more than USD 1.72 billion for 2023, including nearly USD 1.2 billion returned to the Medicare Trust Funds, according to estimations from the U.S. Department of Health and Human Services (HHS). This significant recovery demonstrates the effectiveness and widespread use of fraud analytics in the region.
The Asia Pacific region is projected to record the highest compound annual growth rate (CAGR) during the forecast period. The market's notable advancement is primarily driven by several factors including an increase in healthcare expenditure, growing concern regarding healthcare fraud, and government initiatives to incorporate advanced analytics solutions into the healthcare landscape. Cases of medical insurance fraud grew 15% in Japan in 2023 compared to 2022, according to data from Japan's Ministry of Health, Labour and Welfare. The growth of fraudulent activities is leading the government to invest in advanced analytics solutions, which is adding to the region's swift market growth. In late 2023, China's National Healthcare Security Administration said it rolled out a national fraud detection system that uncovered more than 500,000 suspicious claims in the system’s first six months. This initiative underscores the increasing adoption of healthcare fraud analytics in the Asia Pacific region and corroborates its anticipated high growth rate.
Need any customization research on Healthcare Fraud Analytics Market - Enquiry Now
Key Players
Key Service Providers/Manufacturers
-
IBM Corporation (US) (IBM Watson Health, IBM Safer Payments)
-
Optum, Inc. (US) (Optum Program Integrity, Optum Fraud Waste & Abuse Detection)
-
SAS Institute Inc. (US) (SAS Fraud Framework, SAS Detection and Investigation for Health Care)
-
LexisNexis Risk Solutions (US) (LexisNexis Fraud Intelligence, LexisNexis Risk Management Solutions)
-
Veradigm (US) (Veradigm AccelRx, Veradigm ePrescribe)
-
Feedzai (Portugal) (Feedzai Enterprise, Feedzai Solutions)
-
Change Healthcare (US) (ClaimsXten, Payment Accuracy Solutions)
-
Cotiviti, Inc (US) (Fraud Waste and Abuse Detection, Payment Accuracy)
-
HMS Holdings Corp. (US) (Program Integrity Services, Payment Integrity Solutions)
-
Pondera Solutions, Inc. (US) (Fraud Detection as a Service, FraudCaster)
Users:
-
UnitedHealth Group (US)
-
Anthem, Inc. (US)
-
Aetna Inc. (US)
-
Cigna Corporation (US)
-
Humana Inc. (US)
-
Kaiser Permanente (US)
-
Blue Cross Blue Shield Association (US)
-
Centene Corporation (US)
-
Molina Healthcare, Inc. (US)
-
WellCare Health Plans, Inc. (US)
Recent Developments
-
In November 2024, the U.S. Department of Health and Human Services Office of Inspector General (OIG) published a report assessing the effectiveness of predictive analytics for healthcare fraud detection. The report highlighted a 25% increase in fraud identification when using these advanced techniques.
-
In June 2023, Jack Henry introduced Payrailz Fraud Monitor, a new, cloud-based component of the Payrailz Digital Payments Platform. It recognizes fraudulent transactions in real-time, starting from the point when a payment is initiated.
| Report Attributes | Details |
|---|---|
| Market Size in 2023 | USD 2.36 Billion |
| Market Size by 2032 | USD 17.6 Billion |
| CAGR | CAGR of 25% From 2024 to 2032 |
| Base Year | 2023 |
| Forecast Period | 2024-2032 |
| Historical Data | 2020-2022 |
| Report Scope & Coverage | Market Size, Segments Analysis, Competitive Landscape, Regional Analysis, DROC & SWOT Analysis, Forecast Outlook |
| Key Segments | • By Solution Type (Descriptive Analytics, Prescriptive Analytics, Predictive Analytics) • By Delivery Model (On-premises, Cloud-based) • By Application (Insurance Claim Review {Postpayment Review, Prepayment Review}), Pharmacy billing Issue, Payment Integrity, Others) • By End User (Public & Government Agencies, Private Insurance Payers, Third-party Service Providers, Employers) |
| Regional Analysis/Coverage | North America (US, Canada, Mexico), Europe (Eastern Europe [Poland, Romania, Hungary, Turkey, Rest of Eastern Europe] Western Europe] Germany, France, UK, Italy, Spain, Netherlands, Switzerland, Austria, Rest of Western Europe]), Asia Pacific (China, India, Japan, South Korea, Vietnam, Singapore, Australia, Rest of Asia Pacific), Middle East & Africa (Middle East [UAE, Egypt, Saudi Arabia, Qatar, Rest of Middle East], Africa [Nigeria, South Africa, Rest of Africa], Latin America (Brazil, Argentina, Colombia, Rest of Latin America) |
| Company Profiles | IBM Corporation, Optum, Inc., SAS Institute Inc., LexisNexis Risk Solutions, Veradigm, Feedzai, Change Healthcare, Cotiviti, Inc., HMS Holdings Corp., Pondera Solutions, Inc. |